TRUNK MOVEMENT IN DIFFERENT SEATED PIVOT WHEELCHAIR TRANSFER TECHNIQUES
Karen M. Meess1, Chung-Ying Tsai, MS2,3; Alicia M. Koontz ,PhD, RET2,3;
1Department of Biomedical Engineering, University of Rochester, Rochester, NY;
2Human Engineering Research Laboratories, Department of Veterans Affairs, Pittsburgh, PA;
3 Department of Rehabilitation Science and Technology, University of Pittsburgh, Pittsburgh, PA;
INTRODUCTION
Reaching the optimal wheelchair transfer technique is vital for individuals with mobility impairment in order to maintain independence to perform activities of daily living by reducing the risk of pain and injury. The average wheelchair user performs 15 to 20 seated pivot transfers daily such as: getting into and out of bed or on and off variable height seats for example: shower bench, motor vehicle seat, and commode (Finley, McQuade, & Rodgers, 2005; Gagnon, Koontz, Brindle, Boninger, & Cooper, 2009) . The weight of individuals is supported by the upper extremities (UEs) leading to a force and moment distribution within the shoulder, elbow, and wrist joints. Poor transfer technique has been identified as a risk factor with loss of function of the upper extremities (Nyland et al., 2000). Improper transfer technique increases the risk of injury and pain which are responsible for limitation in activity, increase in health care expenses, depression, and a decrease in quality of life (McClure, Boninger, Ozawa, & Koontz, 2011).
The seated pivot wheelchair transfer (SPT)s utilized by wheelchair users who are unable to stand unsupported (Somers, 2009). The upper extremities support the body weight as a user pivots their body to the target surface. The leading arm, on the transfer surface, pulls the body through lift phase with shoulder abduction, where the trailing arm, on the initial surface, pushes and stabilizes the body weight with shoulder adduction requiring great activation of adductor muscles. This leads to unique force loadings in the UEs (Gagnon, Nadeau, Noreau, Eng, & Gravel, 2008; Kankipati, 2012) .
Many studies have aimed to find the optimal wheelchair transfer technique. A rotational strategy, such as head-hips, with increased trunk flexion, was identified with greater shoulder moments and smaller vertical forces distributed throughout the UEs. Thus it was concluded that the recruitment of larger adductor muscles reduced the risk of injury of rotator cuff muscles with the head hips technique (Gagnon, et al., 2009; Koontz, Kankipati, Lin, Cooper, & Boninger, 2011a)
Although specific transfer biomechanics have been analyzed, wheelchair users tend to utilize their own technique which can be identified as one of the two identified categories of SPTs or a combination of both. o No study has yet tried to classify preferred transfer techniques.
The purpose of this study is to analyze and compare the 3D range of motion and translation movement of the trunk in three prescribed transfer techniques: 1) head-hip relationship with an abducted leading arm away from the body (HH-A); 2) head-hip relationship with an internally rotated leading arm close to the body (HH-I), and 3) with the trunk upright with an abducted leading arm away from the body (TU) (Koontz, et al., 2011). These techniques were derived from the Clinical Practice Guidelines related to best transfer practices (Boninger et al., 2005). The second aim was to use this information to classify the preferred method of transfer employed by wheelchair users.
METHODS
Subjects
Fourteen subjects volunteered to participate in this study and signed informed consent. The inclusion criteria were: spinal cord injury C4 level or below that occurred over one year prior to the start of the study, able to independently transfer to/from a manual wheelchair without human assistance or assistive devices, over 18 years of age, and free from upper extremity pain that influenced their ability to transfer.
Experimental Protocol
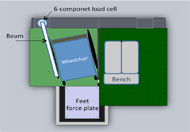
Subjects positioned their wheelchair on an aluminum mounting platform in relation to the target seat which is adjusted to be level with the wheelchair seat and to the subject’s left. The wheelchair and target seat are bolted into a stationary state on the transfer setup as shown in figure 1. Three force plates were positioned under the wheelchair, under the level bench, and under the feet (Bertec Corporation, Columbus, OH, USA). A six component load cell attached to a grab bar was positioned to simulate the user’s wheelchair armrest (Model MC5 from AMTI, Watertown, MA,USA). Coordinate data of markers placed on various landmarks on the trunk with respect to the global reference frame were recorded by a 16 camera motion capture system (Vicon Peak, Lake Forest, CA, USA).
All the subjects started the transfers with their left arm leading (hand placed on the bench) and right arm trailing (hand on placed the beam). Subjects were asked to perform a self-selected (SS) SPT as they normally would for the first transfer. Three transfer techniques, HH-A, HH-I and TU, were instructed to subjects via an informational video. Figure 2 visually shows these transfer techniques. The prescribed transfer approaches were randomly assigned. Subjects were permitted time to practice each technique until they felt they could perform it well. Subjects were then asked to perform these transfer techniques during data acquisition in a random order after practicing. Visual targets guided the subject on hand placement. Five transfer cycle trials were recorded for each transfer technique.
Data Analysis
Kinetic data were filtered using Matlab (Mathworks Inc., Natwick, MA,USA) with a 4th order, zero-lag, low pass Butterworth filter with a sampling frequency of 360 Hz, and a cutoff frequency of 7 Hz (Koontz, et al., 2011a).
A transfer, (wheelchair to transfer surface), was defined as starting upon loading on the right hand grab bar and ending before the impact spike of the buttocks on force plate beneath the transfer surface (Kankipati, Koontz, Vega, & Lin, 2011).
For each transfer the orientation of the thorax coordinate system with respect to the global coordinate reference system was identified with the following four markers according to the International Society of Biomechanics guidelines: sternum, xyphoid process, C7 vertebrae, and T8 vertebrae (Wu et al., 2005) . Using linear algebra and rotation matrices these angles were calculated for the duration of the previously identified transfer period assuming a Cardan angle sequence of Z-X’-Y’’ with respect to the starting thorax coordinate system orientation.
Maximum and range of motion (ROM) of rotation angles (flexion, side bending, and axial rotation) and translations of the trunk (forward/backward, height, and transverse horizontal directions) were calculated for each transfer trial and then averaged over all five trials of each transfer technique for each individual subject. Shapiro-Wilk test was used to test the normality of data. One-way repeated measures was used to determine significance of each variable over the three transfer techniques (TU, HH-A, and HH-I) with Bonferroni adjustment as post hoc test and a level of significance at p < 0.05. SSPS software (SPSS Inc. Chicago, Il) provided the statistical analysis tests required.
RESULTS
Demographics
The sample consisted of thirteen men and one women with SCI level of injuries that ranged from C4 to L1 with 8 incomplete and 4 complete injuries, and 2 unspecified. The group mean (standard deviation) of age, height (in), weight (kg), and years since SCI injury were 38.29(9.76), 50.50(2.93), 72.86(16.57), and 15.42(7.80).
Table 1 shows the results of the trunk movement in the four transfer techniques. Maximum flexion and ROM of flexion/extension for HH-A and HH-I were greater in comparison to TU, with HH-A being significantly greater than TU (p=0.009 and p=0.001 respectively). Maximum right side bending and ROM of side bending for HH-A and HH-I were greater compared to TU, with HH-A and HH-I being significantly greater than TU (p<0.0001 and p<0.0001 respectively). Horizontal translation for HH-A was significantly greater than HH-I (p=0.001).
| TU | HHA | HHI | SS | p | |
| Max Flexion() | 27.88* 5.04 | 41.43* 10.88 | 36.15 13.66 | 29.35 11.48 | 0.009 |
| Max R. Side Bending () | 36.83*, 11.41 | 47.7* 11.70 | 46.14 10.38 | 41.61 11.31 | 0.000 |
| Max R. Axial Rotation () | 38.64 11.39 | 39.71 14.76 | 40.14 19.28 | 41.56 14.70 | 0.792 |
| ROM Flexion/ Extension () | 33.73* 7.05 | 49.61* 17.55 | 41.52 12.43 | 36.13 10.73 | 0.001 |
| ROM R/L. Side Bending () | 41.89*, 10.15 | 50.66* 10.87 | 48.81 8.46 | 44.46 10.24 | 0.000 |
| ROM R/L. Axial Rottaion () | 40.35 10.24 | 45.35 16.83 | 42.71 16.56 | 44.70 10.62 | 0.801 |
| Height (mm) | 108.39 42.14 | 151.02 71.30 | 123.88 43.89 | 111.28 40.91 | 0.036 |
| Horizontal (mm) | 293.37 76.99 | 289.51# 78.04 | 259.24# 116.64 | 261.09 94.22 | 0.001 |
| Forward (mm) | 325.77 89.24 | 360.24 90.18 | 336.09 107.59 | 321.57 101.75 | 0.138 |
*, significant difference between TU and HH-A , significant difference between TU and HH-I #, significant difference between HH-A and HH-I |
|||||
DISCUSSION
HH versus TU Trunk Flexion & Right Side Bending
Both head-hips techniques show significantly greater maximum and ROM of trunk flexion, as well as maximum right side bending and ROM of side bending compared to TU. Both variables quantitatively express how the head and hips rotate in opposite directions during transfer. ‘Head-hips’ (HH), is characterized by increased trunk flexion as the user rotates forward, shifting the center of mass (COM) forward, and using a moment created by the combination of forward flexion and side bending of the trunk to lift and move the hips in the opposite direction of the head (Allison, Singer, & Marshall, 1996). A TU transfer where the trunk and head remain upright, relatively in line with the hips during translation, explains the smaller trunk flexion angles. Thus these two variables are significant in categorizing transfer type.
Smaller vertical forces in all joints of the upper limb were observed for the rotational strategy reducing injury risk. From previous research it has been shown that rotational techniques result in less biomechanical loading in the UEs compared to the translational technique expressed through trunk flexion and after this study, trunk flexion ROM (Gagnon, et al., 2009; Koontz, et al., 2011a) .
Translation ROM versus Transfer Technique
Although not significant, the increased forward and height translation for the head hip techniques shows that the trunk elevates and translates more forward during transfer due to increased trunk flexion and the generated momentum.
Horizontal translation was statistically greater for HH-A in comparison to HH-I, which results from a greater initial distance between the hands with an abducted hand position. The horizontal distance traveled should be relatively equal between TU and HH in the standardized setup (e.g. both used the same hand targets).
Classification of the Self Selected Transfer
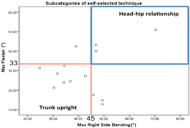 Figure 4: Maximum flexion versus maximum right side bending to characterize HH technique with threshold values.
Figure 4: Maximum flexion versus maximum right side bending to characterize HH technique with threshold values.In order to understand more detail about subjects’ self selected technique, we subcategorize SS into HH-I, HH-A and TU. Maximum and ROM of flexion and side bending were shown to be statistically significant in determining differences between transfer types so maximum of flexion and side bending were used to differentiate transfer type performed in SS transfers first. From this analysis, acceptable threshold values to categorize HH technique based on maximum flexion and maximum right side bending of 33 and 45 respectively which are within the range of one standard deviation from the HH mean but out of the range of TU. Figure 4 shows the relationship of greater flexion and greater right side bending to be associated with HH. Implementing these threshold constraints on the 14 subject SS transfers: 3(21.43%) performed a HH transfer, 7(50.00%) performed a TU transfer, and 4(28.57%) a combination not identified as either.
A good transfer also needs to have shorter translation distance (Boninger, et al., 2005). Therefore, a horizontal translation movement of 260 mm was used to further identify HH-I from HH-A transfers. The threshold was larger than the mean of horizontal movement for HH-I, but within the range of one standard deviation from the HH-A mean. Combining the thresholds in the subjects who used HH in their SS technique, one person utilized the HH-A, and the other two utilized HH-I.
Although currently the HH technique is taught primarily to users with weak triceps and/or high levels of trunk involvement (Sisto, Druin, & Sliwinski, 2008), in our subject population, TU was the preferred transfer technique over HH. Because studies show that upper limb forces may be larger using this TU technique (Koontz, Kankipati, Lin, Cooper, & Boninger, 2011b) it could put someone at risk overtime to developing overuse injuries. Thus it’s important to be able to identify what type of technique a person uses in order to correct those techniques that might be harmful to the person. Our study entailed using motion capture with trunk markers to classify the SS technique, however, because of the dichotomous nature of the classification scheme (e.g. based on threshold angles) it may be possible to judge these angles with a good clinical eye without expensive equipment.
Our study found that the HH techniques also resulted in greater ranges of motion in rotation and translation as the user’s COM translates forward, even more so for HH-A compared with HH-I. These larger movement patterns may increase the risk of placing the user in an unstable position during HH transfer, thus increasing the chance of fall and injury although the motion results in smaller UE loadings. It’s a trade off of transfer techniques with increased loading or increased instability. Therefore, an appropriate transfer technique needs to match the wheelchair user’s physical condition such as muscle strength and trunk control to help them transfer efficiently and prevent injuries.
Study Limitations and Future Work
A key limitation in this study is the small subject population and high variance which may have prevented the significance of other variables to be visible. Also the transfer station is not a natural environment for subjects however they tend to adapt very quickly as they are often faced with many unique types of transfers in daily living. Future work will combine upper limb movement patterns with the trunk patterns to better classify the self-selected techniques.
CONCLUSION
Our data identifies that the HH techniques result in significantly larger movement patterns through trunk flexion and rotations, possibly placing the user in an unstable position during transfer although previous research has indicated that HH techniques result in smaller loadings in the UEs.
If a wheelchair user has the ability to perform the HH technique, the recommended transfer technique should be HH with a close leading hand position. This utilizes HH technique to decrease the loading throughout the UEs while the movement pattern range falls in between HH-A and TU for stability, as the hands and center of mass are kept in close to the body. A classification scheme based on the trunk movement data of prescribed techniques was used to determine what type of SS technique a person uses. This could be helpful in assessing and training or retraining new transfer skills. Future studies are needed to characterize those techniques that did not fit into a particular technique category and evaluate the ability to characterize technique based on a trained clinical eye or using low cost clinical tools.
REFERENCES
- Allison, G. T., Singer, K. P., & Marshall, R. N. (1996). Transfer movement strategies of individuals with spinal cord injuries. Disabil Rehabil, 18(1), 35-41.
- Boninger, M. L., Waters, R. L., Chase, T., Dijkers, M. P. J. M., Gellman, H., Gironda, R. J., et al. (2005). Preservation of upper limb function following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med, 28(5), 434-470.
- Finley, M. A., McQuade, K. J., & Rodgers, M. M. (2005). Scapular kinematics during transfers in manual wheelchair users with and without shoulder impingement. Clin Biomech (Bristol, Avon), 20(1), 32-40.
- Gagnon, D., Koontz, A. M., Brindle, E., Boninger, M. L., & Cooper, R. A. (2009). Does upper-limb muscular demand differ between preferred and nonpreferred sitting pivot transfer directions in individuals with a spinal cord injury? J Rehabil Res Dev, 46(9), 1099-1108.
- Gagnon, D., Nadeau, S., Noreau, L., Eng, J. J., & Gravel, D. (2008). Trunk and upper extremity kinematics during sitting pivot transfers performed by individuals with spinal cord injury. Clin Biomech (Bristol, Avon), 23(3), 279-290.
- Kankipati, P. (2012). Upper limb kinetic analysis of sitting pivot wheelchair transfer techniques in individuals with spinal cord injury. University of Pittsburgh, Pittsburgh.
- Kankipati, P., Koontz, A. M., Vega, A., & Lin, Y. S. (2011). Phase Identification of Sitting Pivot Wheelchair Transfers. Paper presented at the American Society of Biomechanics.
- Koontz, A. M., Kankipati, P., Lin, Y. S., Cooper, R. A., & Boninger, M. L. (2011b). Upper limb kinetic analysis of three sitting pivot wheelchair transfer techniques. Clin Biomech (Bristol, Avon), 26(9), 923-929.
- McClure, L. A., Boninger, M. L., Ozawa, H., & Koontz, A. (2011). Reliability and validity analysis of the transfer assessment instrument. Arch Phys Med Rehabil, 92(3), 499-508.
- Nyland, J., Quigley, P., Huang, C., Lloyd, J., Harrow, J., & Nelson, A. (2000). Preserving transfer independence among individuals with spinal cord injury. Spinal Cord, 38(11), 649-657.
- Sisto, S. A., Druin, E. L., & Sliwinski, M. M. (2008). Spinal Cord Injuries: Management and Rehabilitation (1 Har/DVD edition ed.): Mosby.
- Somers, M. F. (2009). Spinal Cord Injury: Funcitonal Rehabilitation (3 ed.): Prentice Hall.
- Wu, G., van der Helm, F. C., Veeger, H. E., Makhsous, M., Van Roy, P., Anglin, C., et al. (2005). ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion--Part II: shoulder, elbow, wrist and hand. J Biomech, 38(5), 981-992
ACKNOWLEDGEMENTS
This material is based upon work supported by the Department of Veterans Affairs (F4489R) and from the National Science Foundation ASPIRE Grant # B6789C. The contents of this paper do not represent the views of the Department of Veterans Affairs or the United States Government.